AMHA-OR became IMHPA 9/2023
IMHPA Collaboration with Moda Health for VBC, VBP, VBR, MBC, OIC
December 18, 2022
Executive Summary
On October 10, 2022, Moda’s Behavioral Health Director, Dan Thoma, MA, and Jeff Olsgaard, LPC met with Michael Conner, PsyD and Michaele Dunlap, PsyD representing Mentor Research Institute (MRI), a 501c3, to discuss a collaboration agreement concerning Value Based Care (VBC) and Value Based Reimbursement (VBR). Issues included access to services, coordination of care, and outcomes informed care. A subsequent document was shared with us and we were asked to provide a response.
In Oregon, there are a many significant challenges in the delivery of mental health and substance use treatment services related to supply and demand factors. Specifically, demand is greater than the supply of professionals to meet the demand, which has led the State of Oregon legislators to pass legislation to address the importance of assuring mental health parity. (See HR3046). Some Healthplans have responded by increasing the amount paid for various mental health services while other Healthplans have sought to established “narrow networks with incentives” to attend to the mental health needs of members. Other Healthplans have taken a “wait and see” approach in maintaining a status quo to see where the industry goes and if programs such as integrated care models increase access through primary care settings.
Moda has taken an approach to increase the quality and effectiveness of mental health services by promoting Outcomes Informed Care (OIC) that offers financial incentives to professionals to increase access, coordinationof care, and enhance quality. An assumption seems to be that these quality factors will increase efficiency that in turn will increase the ability of providers to see more patients. Historical research on how individuals utilize psychotherapy services call this assumption into question. MRI believes the mental health workforce needs to be expanded, individuals recruited to enter the profession, and current mental health professionals need to be retained. These labor force issues are separate from models of care that include OIC and payment models that incorporate Alternative Payment Models (APM) and Value-Based Payment models (VBP). Thus, Moda’s Behavioral Health Incentive Program and the defined beliefs is limited in addressing the full scope of the issues involved in enhancing access to care and improving quality of care.
AMHA-OR conducted a focus group to expand on beliefs important to mental health and substance use treatment services that include:
Quality-based care, for purposes of private practice psychotherapy, is defined by (a) access, (b) practice processes, and (c) outcomes.
Patient care is patient and provider centric.
In January 2022, MRI responded to a MODA Request for Proposals (RFP). MRI offered a program that incorporated relevant implementation science research. It addressed:
A provider and patient centric approach
Measurement/instrument agnostic (patient and provider centric)
Appropriate provider compensation
A technology platform that reflects ease of use
Training and support that is ongoing
Mentor Research Institute has provided leadership to providers in defining best practices that incorporates outcome informed care OIC utilizing a user-friendly technology platform that facilitates a provider-patient centric model of care. However, equally important is a payment methodology that compensates providers for that expertise and dedication to quality services. Requiring and reporting on utilization of procedures (administering a standardized scale/questionnaire) incurs a cost. Bundling payment for MBC work within billing for psychotherapy CPT codes violate transparency regulations. Thus, MRI proposes a model of reimbursement that increases rates for each of the relevant CPT codes for mental health and substance use services as well as adds a reimbursement for administering a standardized measure using unlisted CPT Codes. This supports State of Oregon mental health parity requirements and the intent of HB 3046.
CONTRACTING SUMMARY
Requirements for Measurement-Based Care with Private Practice Psychotherapists
Collaboration drives innovation in practice and financial models.
A Healthplan must challenge itself to define what is considered “value” in its behavioral health contracts.
Models of practice and workflows are provider centric.
Measurement is provider and patient centric.
Collaboration between payers, providers, and patients is important to achieve equity and quality.
Reimbursement rates need to be competitive.
Access is a function of supply and demand, and opportunity cost.
Measurement-Based Care (MBC) does not address access and is only one aspect of quality-value.
Payment methodologies reflect fee-for-service, case rates, episodes of care rates, per member per month, and added incentive payments reflecting value-based payment (VBP). Payment methodologies need to be clearly defined and transparent.
Contracting for the lowest price is based on payer and provider willingness to agree to those price terms.
MRI and AMHA Oregon prefer to provide quality services at a rate that reflects the expertise and competence of providers.
Contracting requires “good faith” and “fair dealing”.
Psychotherapists need to feel the process of measurement has value in order to genuinely express that measurement will be helpful to patients.
Healthplans should contract with psychotherapists who are member of an incorporated group that can contract on behalf of members. This assures peer-based oversight for standards of practice, consultation, and administrative tasks.
Proposal for Moda Value-Based Reimbursements & Behavioral Health Incentive Program
AMHA-OR is an incorporated member-owned group provider organization whereby psychotherapists may opt in or out of contracts.
Members of AMHA-OR have been trained to use the LightQ EHR and therapist locator.
Providers will be asked to complete screening, progress, and satisfaction measures.
Providers will document that patients were offered a timely appointment.
Psychotherapist members of AMHA will be reimbursed a fixed amount per screening for their time and the use of technology. Using a uniquely identifiable CPT code will (a) avoid unnecessary provider costs, (b) reinforce required administration, (c) reduce error in subsequence analysis, and (iv) reduce expense to the contracting organization (i.e., Healthplans.
MRI recommends Moda collaborate with AMHA-OR to include Associate Licensed Counselors, who have AMHA-OR member supervisors (certified by the State of Oregon) in the Moda contract. This will increase the number of available appointments to MODA members seeking services by 93% in the first year. The Moda access program is permissible in the State of Oregon with AMHA-OR oversight. The AMHA OR Board will assume administrative responsibility for the program, ensure there is qualified clinical supervision, and enforce program policies; supervising supervisors, and auditing Associate Licensed Counselor members of AMHA on a monthly basis to ensure medical necessity of care, standards for documentation is followed, and that treatment is empirically supported.
If the essentials for ethical practice and business operations are met Psychotherapists members of AMHA members will opt-in depending on the reimbursement rate. Psychotherapy services will be reimbursed at a rate calculated by using a Moda multiplier for which the product of the CMS rate is no less than the Oregon Health Plan (OHP) rate for CPT® 90834 code: Psychotherapy, 45 Minutes. The 90834 is most frequently used CPT code and that rate, more than other codes, determines the willingness of a provider to see complex and urgent cases. MRI estimates this to be a minimum competitive for private practice MBC.
The decision to shift priorities and workflow between appointments from a focus on charting and treatment to measurement technology requires (a) work and (b) practice efficiency/expense. and (c) must be rewarding. The reward must be paired closely to a new task (i.e., target behavior). A financial incentive for deliberate action and the anticipation of gaining information that is useful is rewarding. It is also respectful of the psychotherapists time, memorable, ethical and a fortification against the distressing experiences and chronic conditions that psychotherapists encounter. A fixed ratio reinforcement schedule of 1 is the most effective way to change choice behavior; and overcome the resistance to MBC, OIC and FIT.
On October 10, 2022, Moda’s Behavioral Health Director, Dan Thoma, MA, and Jeff Olsgaard, LPC met with Michael Conner, PsyD and Michaele Dunlap, PsyD representing Mentor Research Institute. The following statement was sent by Dan Thoma following an agreement that MRI and MODA would create a non-binding collaboration agreement clarifying Value Based Care (VBC), Value-Based Payments, and Value Based Reimbursement (VBR) objectives:
The Moda Behavioral Health Incentive Program (BHIP) is an opt-in program designed to reward quality of care. It is a combination pay-for-participation and pay-for-performance model, meaning that providers who opt in and participate in the elements of the model will receive a bonus, and if a performance target is achieved then the bonus will be larger.
The program is based on the following shared beliefs:
Coordination, access, and effectiveness are key elements of quality of care
Provider and Moda have a shared interest in coordinated, collaborative care
Provider and Moda have a shared interest in patients’ ability to access care readily, timely, and easily
Provider and Moda have a shared interest in the adoption of evidence-based practices
Extensive research supports the effectiveness of treatment that systematically invites patient feedback on the process of care and patient-reported outcomes (Feedback Informed Treatment [FIT], also variously known as Patient-Reported Outcome Measures [PROMs], Outcome Informed Care [OIC], Measurement Based Care [MBC], etc.)
FIT, OIC, and MBC can readily be incorporated into a wide variety of treatment modalities and clinical paradigms.
The Boards of MRI and AMHA-OR have reviewed the proposed “shared beliefs” above and we note that Moda’s input was solicited.
MRI shares Moda’s expressed beliefs as both aspirational and essential to implement a minimum viable MBC, OIC, FIT program. MRI believes a minimum viable program must also recognize the time, resources, and training necessary to allow psychotherapists to implement evidence-based practices and the requisite technology in a reliable and ethical manner.
Context for Collaboration
In Oregon, there are many significant challenges for the delivery of mental health and substance use treatment services related to supply and demand factors. Specifically, demand is greater than the supply of professionals to meet that demand. That, combined with low reimbursement rates, and payments that vary as much as 50 to 100%, creates significant problems with access to services.
In 2020, the Oregon legislature passed HB3046. That bill requires carriers and coordinated-care organizations (CCOs) to conduct analyses of compliance with mental health parity requirements and report specified data both to the State’s Department of Consumer and Business Services and Oregon Health Authority.
HB 3046 – Mental Health Parity Reporting
All carriers that offer individual or group health benefit plans in Oregon that provide behavioral health benefits are required to submit a completed NQTL Reporting Form and Data Reporting Form to comply with reporting requirements outlined in HB 3046.
Please note, for reports due in 2022 (for the 2021 calendar year's data) the due date is April 1, 2022.
All future years' reports are due annually by March 1.
For more information see:
https://dfr.oregon.gov/business/reg/health/Pages/mental-health-parity.aspx
In effect, HB 3046 legislation requires Healthplans to demonstrate they have contracted with enough mental health professionals to meet the needs of their members and to provide mental health care with assurance of parity. Taken together, those requirements are not achievable because there are not enough treatment providers to meet the demand. Some Healthplans have responded by increasing the amount paid for various mental health services while other Healthplans have sought to establish “narrow networks” and networks with incentives to attend to the mental health needs of certain members. Such narrow networks include managed behavioral care systems that may be owned and operated by Venture Capital (VC) investors. Other Healthplans have taken “wait and see” approaches while maintaining operational status quo to see where the industry goes and whether such programs as integrated care models can increase access through primary medical care settings. Integrated care models in medical settings typically involve screening and treating patients for 1 to 3 sessions; usually no more than 6; then referring on those patients who need more care to non-facility individual psychotherapists and facility affiliated group practices. The opportunity costs are such that Healthplans incentive psychotherapists to serve Healthplans which recognize the financial value of mental health service and patient’s needs.
Moda, in their most recent initiative with MRI, proposes to increase the quality and effectiveness of mental health services by promoting Outcomes Informed Care (OIC) that offers financial incentives to professionals to increase access, increase coordination, and enhance quality. An assumption seems to be that these quality factors will increase efficiency that will increase the capacity of providers to see more patients. Historical research on how individuals utilize psychotherapy services calls this assumption into question.
MRI believes the mental health workforce needs to be expanded, people recruited to enter the profession, and that currently active mental health professionals need to be retained. Labor force issues in Oregon are separate from models of care that include OIC/FIT, payment models that incorporate Alternative Payment Models (APM), and from Value-Based Payment models (VBP). Thus, Moda’s Behavioral Health Incentive Program and the beliefs set forth have limitations, not fully addressing the range of issues involved in enhancing access to and improving quality of care. A comprehensive plan to meet access and quality objectives was included in the January 14, 2022, proposal submitted by MRI to Moda.
Mentor Research January 14, 2022 Proposal
Mentor Research Institute (MRI) has worked with Healthplans over the past eight years to enhance the quality of behavioral health services. During the past twenty-five years MRI has offered clinical training to mental health and substance use treatment professionals across Oregon. In 2019 MRI Board members provided an all-day education event focused in part on use of outcome measures to inform clinical practice. We have learned that effective training must start with the lowest dose possible and titrate slowly watching for side-effects (i.e., psychotherapist distress and objections).
Adoption of MBC and OIC in Oregon is less than 5%, based on our survey of Oregon psychotherapists. Models developed for incorporated group practices and public health facilities are dropped when professionals enter private practice. MRI found that when therapists whose employers required measures such as ACORN and MyOutcomes move into solo or group private practice, they often avoid measurement because they do not find the required tools useful.
Since 2018, Mentor Research Institute (MRI) has been training psychotherapists to use the current version of MBC and OIC software developed by Private Practice Cloud (PPC), which offers MBC and OIC, a charting system, a practice analytic dashboard, and a population/group analytic system (Tableau). However, adoption of OIC is not likely when required by a health plan. MRI believes that the level of moral injury and distrust in the U.S. Healthcare industry is so great that anything less than full recognition of provider needs will diminish adoption of MBC and OIC. Providers’ adoption of MBC and OIC must be based on clear benefits that inform work with a specific patient and have low administrative burden.
For more information see:
Moda Outcome-Informed Behavioral Healthcare Proposal
January 14, 2022
By Mentor Research Institute
https://www.mentorresearch.org/private-practice-contracting-for-psychotherapy
While recognizing Moda objectives, psychotherapists want to have control of the services they offer their patients and to be paid a fair reimbursement. In a free market, psychotherapists are paid for service according to supply and demand. When the demand is high and reimbursements are not competitive, psychotherapists may (a) terminate contracts with Healthplans, (b) limit their case-mix severity, and (c) choose patients who are willing to accept “out of network” expense or pay out of their own pockets.
Venture Capital Narrow Networks: Mental Health Service
The impact of Venture Capital investors on mental health services and the public should not be minimized. Managed mental health and MBC services are available to Healthplans and consumers from companies infused by venture-capital investors who demand large profits based on inflated valuations and investor expectations.
New Venture Capital (VC) companies have recently emerged. These million and billion-dollar digital platform companies compete for patients with independent-practice mental health professionals. Venture Capital (VC) companies have marketing and advertising resources private practice clinicians do not. The VC companies have come into the market to employ therapists, to compete with Healthplans for employers’ dollars, or to serve Healthplans, or hope to be purchased by Healthplans. How many of these VC companies have Healthplans among their investors is not clear.
Some new VC companies, offer mental health providers digital services including billing, assessment, appointment scheduling, and teletherapy portals while they also offer the public prescription services, coaching, text or email contacts, counseling, and brief psychotherapy.
Digital mental health services funded by venture capital cannot be just “successful.” They must WIN BIG or will fail because of the high investor-expectations they create.
The only way that huge profits can happen requires the VC companies to take control of psychotherapy services, reduce psychotherapists’ fees-for-service and/or increase the number of patients treated in brief episodes. VC companies cannot afford to address psychotherapists’ ethics, values or the importance of relationships created with clients. VC companies will not hesitate to create policies that risk moral injury on patients and psychotherapists. Psychotherapists are responsible for the policies they follow, not VC companies and Healthplans.
Can VC increase access to care, improve outcomes, coordinate care with physicians and make required profit at the same time? What will happen to patients and employed therapists when a VC company fails or is purchased by another company?
The increase of profits and value that these VC companies seek depends upon their convincing therapists to leave independent practices and become employees of the VC companies.
For more information see:
How Psychotherapy Practice is Being Transformed to High-Profit Managed Care
https://www.amha-or.com/private-practice-is-transformed-to-highprofit-managed-care
As a result of health care reform, and increases in Venture Capital investment in mental health services, Healthplans want psychotherapists to adopt Value-Based Care. There are numerous challenges in adopting VBP for mental health and substance use treatment services since much of VBP is based on overall health care costs as well as a variety of process measures, such as readmission rates following a surgery. As Pincus and Fleet (2022) note there is no clear leadership in developing metrics and moreover, a large component of the workforce are professionals in solo/small practice groups with limited capacity or desire to participate in VBP. Williams, et al (2022) also noted the lag in development of pay for performance (P4P) measures in mental health and substance use treatment services. At this time, participating in value-based payments with Moda is a good idea that requires greater specificity in the relationship of processes and outcomes to what is valued.
Value-based care is a form of reimbursement that ties payments to health system for care delivery to the quality of care provided and rewards providers for both efficiency and effectiveness. The terms value-based payments (VBP) can be used to means payments for episodes of care and/or outcomes, specified in a contract. Under a volume-based pay model, a health system could be compensated for an episode of care and then compensated again if the patient needs additional treatment. With a value-based care approach, health systems are given compensation a single time, and would not be compensated for subsequent care.
More than 40 years of research provides convincing evidence concerning why and how psychotherapy works and clarifies the problems when it doesn’t work; regardless of the type of psychotherapy used. In private psychotherapy practice, VBCs are better described as value-based reimbursement (VBR).
A value-based contract (VBC) for Independent Psychotherapy Practice is a contractual agreement between a Healthplan and psychotherapists where reimbursement for services is contingent on mutually agreed requirements. The requirements may include clinical circumstances, patient outcomes, and/or specified measures of appropriate, timely and effective services. Rather than payment being based on the quantity of service provided (i.e. number or length of sessions), payment is determined by the value of care delivered.
For more information see:
What is Value-Based Contracting (VBC) for Independent Psychotherapy Practice?
https://www.amha-or.com/value-based-contracting-for-independent-psychotherapy-practice
Toward Value-Based Reimbursements (VBR) - MBC, OIC and FIT
An alternative to the Narrow Network payment model would be to promote VBR and Measurement-Based Care (MBC), also referred to as Outcome Informed Care (OIC) or Feedback Informed Treatment (FIT). Healthplans suggest they might increase fees-for-services for psychotherapists who can adopt and implement this model of care. There are problems. Unfortunately, Healthplans don’t know how to adopt and implement a reimbursement model that incorporates MBC, OIC, FIT. Issues include specific details about what constitutes MBC. As an example, adopting FIT as promulgated by Scott Miller requires administering the Outcomes Rating Scale (ORS) and the Session Rating Scale (SRS) at each session. Adopting Patient Reported Outcome Measures (PROMs) as outlined by Jeb Brown would require administering the GAD7 and PHQ9 at each session with 5 rather than the 4-response primary care option. While another therapist adopting the Treatment Outcome Package (TOP; D. R. Kraus, Seligman, & Jordan, 2005) might administer the measure at the beginning of treatment and not again until 5 or 6 sessions later. Yet, another therapist might adopt an Ecological Momentary Assessment in which a daily question is sent to a patient’s mobile device. Psychotherapist members of the American Mental Health Alliance-Oregon (AMHA-OR) use questionnaires such as an ACE, GAD7, PHQ9, PHQ15, MDQ13, as well as a clinician developed, expanding library of questionnaires that measure other symptom and functional problems associated with such clinical concerns as PTSD, ADHD, Substance Use, OCD, Self-Compassion, Patient Satisfaction and Alliance.
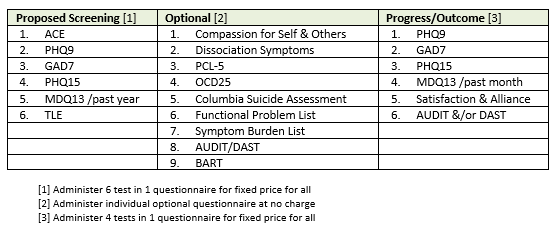
Table 1 provides samples of the questionnaires that are currently available. Each modality may be of value and encompass MBC. Aside from the choices of measures the principle of patient and provider centric care is the important factor in establishing an MBC model. The selection of questionnaires can be created, added to, and modified for differing MBC objectives and targets.
Table 1. Screening, Optional & Progress/Outcome Measure Examples
In moving to VBC, VBP, VBR, a Healthplan must challenge itself to define what is “valued?” Value might be defined as reduced health care service utilization, a return on investment (ROI) or it may be measured as improved health and well-being. Several metrics are possible but many of the VBC, VBP methods in health care require a “shared risk” approach in which a treatment episode is defined, and where the provider is paid for that episode of care; having responsibility for the intensity of services to be provided. Britton (2022) proposed such a model in which a provider is paid for an episode of care. For example, 12 months of treatment for a person with a substance use disorder to provide whatever level of care is needed. For most mental health professionals working in solo practice or in small practice groups shared risk would be devastating financially However, there might be modified aspects of such an approach that could be piloted.
In June 2015, AMHA-OR proposed a model for individual provider contracts with Moda (and another Healthplan) for which therapists in 3 regions of Oregon formed an association and agreed to use (a.) a common EHR, (b.) a formal MBC model, and (c.) co-created integrated analytic analysis and reporting software. That model included use of patient reported outcome measures (PROM) for comprehensive mental health screening, selectable progress measures, and therapist-patient alliance measures. AMHA-OR providers gathered data for nearly a year before presenting their results to several Healthplans.
In June 2018, AMHA-OR proposed a model for individual provider contracts with Moda for which therapists would, for example, treat anxiety and panic for an average of 7 sessions with a 50% reduction in symptom burden as the target value. Reporting involved statistics including the average number of sessions, symptom reduction and effect size.
On January 2022, MRI responded to a MODA Request for Proposals (RFP). MRI offered a non-profit solution adopted and created by mental health professionals in Oregon that incorporated relevant implementation science research. MRI stated that without appropriate provider compensation, and provider leadership, MRI was certain adoption of MBC, OIC and FIT in Oregon would be low and represent large financial loss for private practice psychotherapists. Financial compensation for the added value of MBC, OIC and FIT must account for the administrative costs and the opportunity cost of forgoing treatment of patients with different Healthplans. There are Healthplans in Oregon that offer fee-for-service that are much greater than Moda’s. MRI stated that psychotherapists would not agree to a narrow network contract if required to use a venture capital administered MBC platform.
In October 2022, MODA asked MRI to propose an MBC, OIC, FIT contract that would include incentives for adopting MBC for targets (not yet defined). For illustrative purposes, MRI created a range of options based on financial limitations and outcome measures. There are challenges with one proposed Moda requirement that the cost of MBC, OIC and FIT be included as part of a negotiated rate increase across Psychotherapy CPT codes (e.g., 90791, 90837, 90834, 90839, 90840). MRI understood this would be compensation for implementation, data gathering, aggregating, analyzing, and possibly reporting information to Moda.
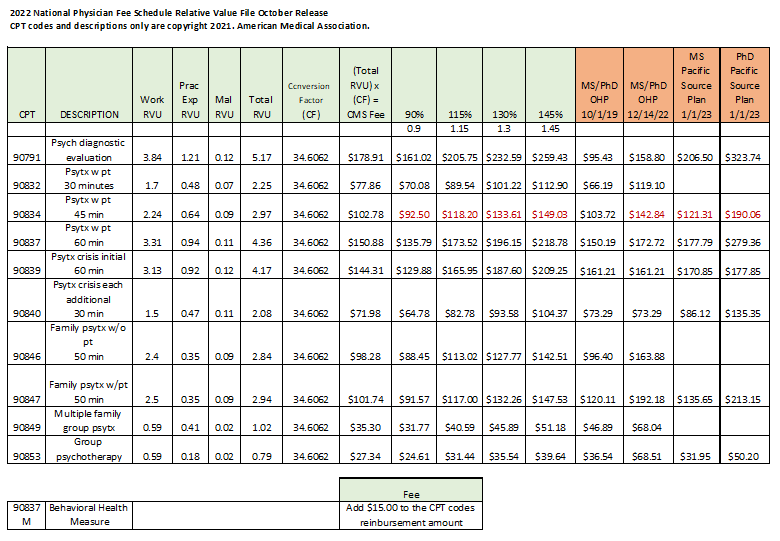
Payment and Reimbursement Challenges: CPT Codes
Historically, Healthplans have contracted for payments using variable code rate schedules (VCRS). The Oregon Health Plans (OHP) sets and periodically adjusts payments for specific CPT codes. Beginning December 14, 2022, the Oregon Health Plan increased their rates (see Table 2). Rather than following the OHP rate example, commercial Healthplans are moving away from code-based fee schedules to payments based on CMS using the Relative Value Units (RVU) and a Conversion Factor (CF) and adjusting the product by percentage multiplier set by the Healthplan. (See Moda example in Table 2).
What are RVUs and CFs? RVUs are used by Medicare to determine the amount of reimbursement to providers based on the provider’s professional status. RVUs are basically a way of standardizing and comparing service volumes across continuums of care. An RVU is an apportionment of cost set by Medicare to determine the amount to pay care providers, dependent on their productivity. It is a number that defines the volume of work providers perform when treating patients for all procedures and services covered under the CMS Physician Fee Schedule. RVUs reflect the relative level of time, skill, training, and intensity required of a physician to provide a given service. RVUs are a method for calculating the volume of work and cost expended by a physician in treating patients. A conversion factor (CF) is a dollar amount used to multiply the RVU (in the Relative Value Schedule) to arrive at the maximum allowable payment for that procedure. The CF is set by Congress and is changed periodically.
RVUs are calculated as three factors, (a) provider work, (b) practice efficiency, and (c) malpractice costs. There is a problem. The RVUs for private practice psychotherapists, which are used to calculate the exact CMS reimbursement rate cannot be used to account for the cost of training and technology, and changes in practice workflow in a psychotherapy practice (to adopt VBC, VBP, OIC, FIT). There is a different schedule that can be applied to facilities such as residential treatment, psychiatric hospitals, and integrated care clinics settings. RVUs for facility-based services do not align with the work, practice, and malpractice RVUs for private psychotherapy practices.
What are Geographic Practice Cost Indices (GPCI)? A geographic practice cost index (GPCI) has been established for every Medicare payment locality for each of the three components of a procedure's relative value unit (i.e., the RVUs for work, practice expense, and malpractice). With the goal of achieving fair and equitable psychotherapist compensation, CMS incorporates a geographic practice cost index (GPCI) into the RBRVS to neutralize regional economies. An RVU must be multiplied by a dollar conversion factor (CF) to become a payment schedule. Medicare calculates an annual CF based on the previous year’s CF and adjusts to maintain budget neutrality. In other words, the GPCI is intended to reflect a difference in cost on a regional basis. In a market such as Oregon, Healthplans that are using CMS to calculate rates are omitting the GPCI and instead use what appears to be an arbitrary multiplier in their calculations to establish rates.
There are problems. Combining measurement work within a psychotherapy CPT code (a) obscures the work practice efficiency processed, and malpractice costs, (b) conflates a psychotherapy service with a host of measurement services, and (c) requires uniform behavioral health data gathering, aggregation, analysis and reporting technology that is impossible to implement across other Healthplans and healthcare professions.
Having examined existing MBC platforms for a decade, and having collaborated in developing two platforms, MRI found that the data gathered for MBC cannot be analyzed at low cost unless there is a CPT code for each measurement service: making measurements a variable of the analyses. Moreover, VBC and VBP can only be achieved in the next decade if Healthplans acknowledge that behavioral and mental health screening, progress, and other assessments are services, separate unto themselves, which require their own CPT codes.
This is important. If the conclusion of an analysis of a quality improvement is based on measurement, and the measures are obfuscated within CPT, the independent variables are obfuscated, and that is large source of error. Also, either the CPT requires a modifier, or a special CPT service code must be used to identify what might be influencing outcome. It would be technically challenging and expensive, or impossible to determine, based on data, to know why targets were or were not achieved. Psychotherapists and Healthplans cannot make data informed decisions unless measurement service are clearly defined and are identifiable in the data set.
Behavioral health measures are analogous to medical imaging, laboratory results, pathology reports, etc. They are mental health vital signs that measure physical, mental, behavioral, and emotional symptoms, and functional burdens.
The challenges facing private practice psychotherapists and the need for a solution to the behavioral health crisis in Oregon require measurements that allow providers and programs to identify and monitor progress toward a target, the value of the target, the investment, and risk. This requires patient and provider reported measures across many patients and entire episodes of care.
Table 2 is presented as an example of what private practice psychotherapists would consider an easy, efficient, and sensible way to implement MBC, OIC and FIT into their daily workflow. Notice that this example documents the RVUs, CF, the CMS rate, and the use of multipliers to adjust CMS rate to compete with other Healthplans. In this example a fixed cost is specified for the use of an outcome measure. For example, $15.00 would be added to the CPT code if a modifier is used to designate that service Psychotherapy & Measurement (P&M). Alternatively, the measurement might be a CPT code that is billed separately as a unique service. The latter is preferable as it would be the least complex to implement, can be internally auditing, and will reinforce the deliberate use of measures. Measurement types would include a screening measure, progress measure, an outcome measure, a patient-provider alliance measure, a medication adherence or side effect measure, or a consumer satisfaction measure. The example used in the outcome measure in Table 1 would be a 90837 with a modifier -99 added to the outcome measure for that appointment (e.g., a 90899).
New services or procedures that do not have an accurate, descriptive CPT or HCPCS code must be reported to payers using an unlisted code. Private payers may reimburse claims with unlisted codes; however, they may determine payment based on their fee schedule for a comparable procedure or other methodologies.
For all their complexities, submitting claims with unlisted codes will help keep you compliant and alert to the need for new CPT codes.
Common documentation requirements include:
A complete description of the nature, extent, and need for the procedure.
A procedure report.
A comparable service or procedure code.
Unlisted codes provide the means of reporting and tracking services and procedures until a more specific code is established. These may be used in commercial billing provided their use and the fee is specified in the payer and provider contract.
Medicare claims using unlisted codes must be accompanied by specific information about the service and/or procedure and supporting documentation. That documentation varies by payer. Billing/claims staff should understand each payers’ process for submitting claims with unlisted codes.
For more information see:
https://nationalascbilling.com/articles/the-business-of-unlisted-codes-strategies-to-avoid-rejections-denials-and-audits/
Table 2. Rate Example for MBC, OIC, FIT for Private Psychotherapy Practice
For more information see:
https://www.cms.gov/medicaremedicare-fee-service-paymentphysicianfeeschedpfs-relative-value-files/rvu22c
It is reasonable to assume that the Oregon Health Plan (OHP) has acceptable rates for their providers in Oregon. Whether or not psychotherapists withdraw from, keep, or sign new Moda contracts will depend upon what Moda offers for the expected work and outcomes for specific targets (Yet to be proposed by Moda). In order to successfully implement MBC, OIC and FIT, MRI recommends an adjustment of at least 150% of CMS for Psychologists and 145% for master’s level counselors and therapists for the basic level of participation in MBC, OIC and FIT. This would be competitive with OHP rates and would likely meet mental health parity requirements, and likely increase the size of Moda’s network. Alternatively, Moda might consider offering a CMS equivalent of 110% of the OHP standard rates to provider groups committed to MBC. What the market will bear is uncertain because providers’ appointment calendars are filled, and demand is outpacing supply. Moreover, psychotherapists are experiencing burnout by the increased number of mental, emotional, behavioral, and physical problems to be dealt with that result from COVID, inflation, and civil and political unrest. MRI believes it is likely that psychotherapists will withdraw from Moda contracts because Moda’s proposed rates, compared to OHP rates, will not be perceived as good faith and fair dealings. Psychotherapists can argue that Moda’s contracting is not sincere regarding their commitment to quality improvement, mental health parity legislation (HB 3046) and ensuring access to services
Access, coordination of care, and effectiveness are separate outcome targets (i.e., separate dependent variables) and can have negative interactive effects based on (a) case mix-severity, (b) location, and (c) availability of providers. For example, patients in low socioeconomic areas are severely distressed, have financial difficulty with co-pays and deductibles, and have difficulty finding providers with available appointments who accept Moda. Coordination of care can be complicated and requires psychotherapists to spend case-management time outside appointment hours. To address these challenges Moda could consider adding an Interactive Complexity CPT Code (90785). MRI supported a survey on behalf of Moda providers that gathered information about the amount of time psychotherapists spend outside of appointments. Many providers work only with patients who do not require complex interactive services not covered by a psychotherapy code.
There is a simple, transparent solution which ties services and costs to outcome targets and recognizes that the work of psychotherapy is very helpful, can be lifesaving, and inflicts an emotional cost to providers. This solution addresses (a) psychotherapist reluctance to implement measures, and (b) payers’ need to calculate bonuses for providers who opt in and participate or larger bonuses for ”achieved performance” targets. At this time a risk-share contract is not possible; Psychotherapists must first adopt MBC and integrate that into their practice workflow.
Based on our research and interactions with thousands of psychotherapists, MRI proposes that the most achievable and efficient way to involve psychotherapists in VBR is for therapists to be paid a fixed price for each screening and progress questionnaire administered. After speaking with a certified fraud examiner MRI concluded that provider-payment of a fixed price should cover the price of administration and the required technology. The cost of interpretation could be included as a rate increase in psychotherapy CPT codes
Since 2015, AMHA-OR has funded and co-created online technology capable of supporting VBC, VBP, VBR, MBC, OIC and FIT. The software offers a library of medical and behavioral health questionnaires and feedback tools. The application delivers screening instruments, provider alerts, on-track treatment reports, measures of treatment alliance and satisfaction and of patient outcomes. This software is designed to be simple, inexpensive, secure and provides basic analytics. A more sophisticated system has been created for MBC, research, and quality improvement. However, Healthplans want providers to use platforms that they control, with dashboards that display patient measurement data.
A focus group held by AMHA concludes that payment greater than $15 per assessment will engage a proportional number of providers to measurement. However, a reimbursement of $15 alone is not sufficient to engage providers in MBC. The example in Table 2 illustrates a feasible provider path to MBC, eliminates the expense and complexity of contract negotiation, maintains accountability of CPT codes, and avoids all antitrust issues. What Moda offers is up to Moda. Whether or not psychotherapists agree to contact is up to those providers. The basis for a decision to participate can be made in “good faith” and “fair dealing.”
Since MBC, OIC and FIT are not incorporated in CMS RVUs, MRI recommends against a Healthplan multiplier to establish fee schedules for MBC. Doing so could be perplexing for auditors when comparing CPT codes among Healthplans, facilities and providers. Using separate CPT codes for measurement is recommended to provide the necessary clarity and transparency. Further, when CMS rate calculation methods are used to establish rates, provider reimbursements increase each time the Federal Government increases the conversion factor. This will not happen if a Healthplan or facility establishes their rates with a multiplier of a CMS reimbursement rate.
Inherent in a contract with Moda is patient-provider appropriate use of data. This has value to everyone. AMHA-OR has access to many clinically useful questionnaires and, in collaboration with MRI, will implement additional measures that are of value to patients and psychotherapists.
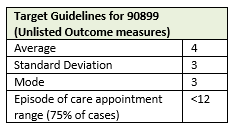
There are significant advantages to a VBR contract that pays per measure. It simplifies contracting deliverables and eliminates hidden and unreliable cost estimates. There is one challenging caveat: Moda would need to create one or more billing codes to be submitted for each measure administered. Or Moda might create 3 codes for (a) Screening, (b) further diagnostic, and (c) outcome measures. Expectable measurement patterns might be 1 to 7 measures over a typical 7 to14 session patient encounter. Seven measures would be about half the cost to the payer of one treatment appointment. Table 3 illustrates an Outcome Measurement Administration Guideline proposed by MRI. For longer treatment episodes, measures of symptom burden or functional problems would be expected to support the medical necessity of services.
Table 3. Outcome Measurement Administration Guideline Example
Moda would also need psychotherapists to use software that documents psychotherapists’ use and analysis of measures. Measurement dates will be captured by Moda as part of psychotherapists billing. This will allow Moda to track who and who is not using measures without requiring provider time and expense to aggregate and report seperately. AMHA-OR members, as an example, already have the necessary software to administer, document, and aggregate data, and have participated in its development. There are other vendors who can provide the necessary technology; depending on Moda reimbursement offer. Psychotherapists will need training to ensure that they understand the focus of a VBR contract to ensure they do not manipulate the contract. MRI can provide that training. Working with Moda, MRI can also provide anonymous reporting with feedback to psychotherapists who are part of the Moda network.
Transparency and Shoppable Services
Healthcare in Oregon is struggling to create Alternative Payment Methods (APM) for behavioral health. This struggle is most apparent in the disconnect between Oregon’s Measure 110 and access to treatment for substance use and mental health disorders. Among the obstacles to quality improvement in Oregon have been Antitrust Laws and Federal Trade Commission guidance that forbid facilities and psychotherapists from gathering, aggregating, and analyzing costs and reimbursements across Healthplans. Inability to know what Healthplans are reimbursing others for services has prevented facilities and private practice psychotherapists from proposing and analyzing VBC opportunities. Contracts offered by Healthplans in Oregon have tight financial margins; and there is significant waste and inefficiency. The perceived risk of APM is high and the rewards may disproportionately benefit Healthplans.
The Transparency in Coverage Final Rule will be a significant help to enhance quality in private practice psychotherapy. Every insurance company and self-insured company must now share all the rates they have negotiated with providers (doctors, hospitals, etc.). This transparency makes Healthplans and practitioners each more accountable, which can lead to better patient outcomes and value.
Beginning July 1, 2022, most group health plans, and issuers of group or individual health insurance coverage are required to disclose, on a public website, machine-readable files containing in-network rates for covered items and services and allowed amounts and historical billed charges for out-of-network providers.
Making pricing information publicly available strengthens the work of health care stakeholders that provide care, promote access to care, or otherwise aim to protect consumers and the health care system. These entities include researchers, regulators, lawmakers, patient and consumer advocates, and businesses that provide consumer support tools and services.
With information on pricing, these health care stakeholders can better fulfill each of the unique roles they play to improve America's health care system for consumers. For example, with pricing information, researchers can better assess the cost-effectiveness of various treatments; state regulators can better review issuers' proposed rate increases; patient advocates can better help guide patients through care plans; employers can adopt incentives for consumers to choose more cost-effective care; and entrepreneurs can develop tools that help doctors better engage with patients.
For more information see:
https://www.cms.gov/healthplan-price-transparency/public-data
By January 1, 2023, plans and issuers must make price comparison information available with respect to an initial list of 500 identified items and services. By January 1, 2024, plans and issuers must make price comparison information available with respect to all covered items and services.
For more information see:
https://www.cms.gov/healthplan-price-transparency/consumers
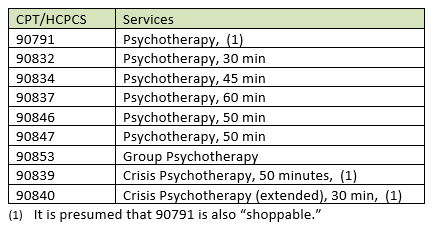
According to CMS, psychotherapy services are considered “shoppable services,” meaning the public should be provided with a good faith estimate for the cost of services prior to their first appointment. Psychologists and other health care providers are now required by law to give uninsured and self-pay patients a good faith estimate of costs for services that they offer. The applicable psychotherapy services are displayed in Table 4.
Table 4. – Shoppable Services
For more information see:
https://www.cms.gov/CCIIO/Resources/Regulations-and-Guidance/Downloads/CMS-Transparency-in-Coverage-9915F.pdf
Price Transparency aims to give patients and consumers a clear sense of what upcoming health care services will cost. All this information is available to the public, Healthplans, researchers, and technology developers. Psychotherapists can gather, aggregate, analyze and report this information because it benefits consumers and because it is pro-competitive. Psychotherapists can now talk among themselves because Healthplan rates are no longer proprietary and subject to confidentiality agreements. As always, providers who do not share a common Tax Id cannot come together and/or communicate for the purpose of setting or bracketing reimbursement rates; nor can they collectively agree to boycott a payer or Healthplan. To do would be a violation of Federal Trade Commission (FTC) regulations.
Good Faith and Fair Dealing in Contracting
Do psychotherapists have a legal and ethical responsibility to NOT participate in a contract if the psychotherapist expects they will disproportionately serve more patients covered by a Healthplan that pays more? If contracts are equivalent in their expectations, the simple answer is yes. According to the American Bar Association…
In general, every contract contains an implied duty of good faith and fair dealing. This duty requires that neither party will do anything that will destroy or injure the right of the other party to receive the benefits of the contract.
“Good faith” has generally been defined as honesty in a person’s conduct during the agreement. The obligation to perform in good faith exists even in contracts that expressly allow either party to terminate the contract for any reason. “Fair dealing” usually requires more than just honesty. It requires that a party cannot act contrary to the “spirit” of the contract, even if you give the opposing party notice that you intend to do so.
It is important that you and your business understand what your obligations are under a contract—not just the actual contract terms, however, but also the implicit terms, like the duty of good faith and fair dealing. This is because, during a contract, if the other party asks you for help and you do not provide it because the contract terms do not require you to do so, you may have unintentionally breached the agreement.
Whether you are about to enter into a contract or are already a party to numerous agreements, talk to an attorney to understand what the duty of good faith and fair dealing requires of you and your company.
For more information see:
https://www.americanbar.org/groups/litigation/committees/business-torts-unfair-competition/practice/2016/duty-of-good-faith-fair-dealing/
In contract theory and economics, information asymmetry deals with the study of decisions in transactions where one party has more or better information than the other. Asymmetric information is, just as the term suggests, unequal, disproportionate, or lopsided information. Contracting with Healthplans involves asymmetric information. Healthplans have more information than an individual psychotherapist or a group of psychotherapists. In certain transactions, Healthplan contracts could take advantage of psychotherapists because asymmetric information exists.
An ethical and justifiable contract would require a trade of goods and service (i.e., health care) for money (i.e., reimbursement for services) and that each party not withhold information that would otherwise result in either party failing in their ability to fulfill the contract. No party should withhold information that would otherwise result in harm such that the other party would make a different decision to prevent harm.
Does the legal principle of good faith and fair dealing require a psychotherapist to see patients who have a lower paying Healthplan as willingly as they engage with patients who have a Healthplan that pays more? The answer is yes.
Does the legal principle of good faith and fair dealing require a Healthplan to offer psychotherapists a reimbursement rate that the Healthplan knows will probably result in the therapist admitting that patient to their practice? The answer is yes.
How will a Healthplan know they are violating principals of good faith and fair dealing? They will know it because (a) they are paying psychotherapists significantly less than other health plans, (b) demand for psychotherapists is greater than the supply, and (c) patients are not finding the medical and mental health services they need in a timely manner.
It is worth noting again that as a result of the Oregon’s Mental Health Parity Law (HB3046) the State will be analyzing data provided by Healthplans including reimbursements, Healthplan membership, and network size. Information to identify which Healthplans are not adequately serving their members will be available publicly.
Should a psychotherapist enter a contract with a Healthplan that is not offered in good faith? The answer is no.
Quoting a certified fraud examiner who was consulted: “90% of a contract rate that is crap (i.e. not competitive), is still crap.” The fact that the contract that was offered is “crap” is also not justification for not providing service to people seeking health care services. Yet many psychotherapists sign contracts knowing they are less willing and are unlikely to accept new clients from Healthplans that have low reimbursements.
In November, Moda offered a new contract with a reimbursement rate that is calculated as the product of multiplying CMS rate times a percentage that is set by Moda. Providers, depending on their profession (and not their value), are paid more or less than the CMS rate. Moda is also reimbursing counselors and social workers significantly less than psychologists. There is, however, no evidence that psychotherapists with a master’s degrees are less effective than those who have doctorates. The assumption that psychologists are better psychotherapists than providers with a master’s degree is popular belief among Healthplans, there is evidence that the opposite may be true.
Does a Healthplan harm the public by negotiating a contract with providers for a low rate for a network that already has too few providers to responsibly serve their plan members? The answer is yes.
• Do health plans know the psychotherapist and Healthplan sre acting in bad faith? yes.
Oregon has reached supply and demand discrepancy with large rate discrepancies that a Healthplan can reasonably be expected to know they are making a deal that is too good to be true.
Who is harmed when Healthplans and psychotherapists agree to contracts in bad faith? The employer is defrauded. The must go without timely service or must pay for services out of their own pocket.
There is good news for employers, patients, and psychotherapists. As a result of the Transparency in Coverage regulations effective January 1, 2022, employers and patients seeking care can estimate if they are likely to access mental health services more or less than another Healthplan. Table 2 helps to illustrates why people will find it difficult to find a psychotherapist and access mental health services.
Why would a Healthplan offer a rate so low that their members will be disproportionately underserved (i.e. denied services because their coverage is not reimbursed on par with that of other patients with the same needs)? Here are 3 considerations.
The quality of care is not driven by accountable and evidence-based quality improvement programs. Quality of care is usurped by the Healthplan’s Contract profit objectives. The contracting department is ultimately controlled by the Chief Financial Officer. The Healthplan’s Behavioral Health department has authority to propose a quality improvement program, but insufficient authority to fund it.
The purpose of the contract is to maximize profit and minimize short term risks to the Healthplan. Patients who are dissatisfied with their inability to access services either (a) leave the Healthplan, or (b) tolerate the consequences of not receiving treatment. Healthplans have a culture of cutting costs rather than investing to be more efficient and of restraining access to behavioral health services.
Healthplans know that providers may sign a contract but take no action to ensure patients have access to care on par with that of the provider’s other contracted Healthplans. Healthplans may blame providers for acting in bad faith rather than offering contracts in good faith that are fair and transparent to consumers.
Providers may sign poor-paying contracts. Three common reasons are because (a) they want to provide clinical services, (b) they are specialized or have a professional interest in working with certain mental health patients and/or problems, or (c) they have reciprocal referral arrangements with other professionals. But they are not willing to ruin themselves financially. Unless exceptions like these are explicit in a contract, Healthplans and psychotherapist risk accusation of committing fraud.
An ethical contracting group will not enter into contracts that are not in good faith. For example, there is The American Mental Health Alliance – Oregon (AMHA-OR), a non-profit corporation. AMHA-OR supports these principles…
People have the right to choose their own therapists.
Psychotherapy is a collaborative process between therapist and client in service of the client.
Therapists shall preserve client confidentiality.
Mental health professionals shall create an interdisciplinary community that promotes and supports competent and ethical practice.
In 2016 AMHA-OR adopted “Ethical Principles, Practice and Business Operation for Collaborative Mental Health Services.” Psychotherapists agree to follow these as a condition of membership. Fundamental Principles and Guidelines for Professionals Engaged in Business Operations:
Beneficence and Non maleficence
Full Awareness
Acceptability
Monitoring and Accountability
Refusal to Condone and Participate
For the professions of psychology to fulfill their potential, mental health professionals must uphold public trust in the professions’ ethical and scientific integrity across all domains. Some activities that fall within the field of operational psychology carry a high risk of undermining public trust and professional integrity, thereby diminishing the reputation and effectiveness of the mental health professions.
Psychologists and mental health professionals have a duty to refuse to condone and participate in activities that will substantially violate their professional ethics, and they must have realistic opportunities to do so. However, some mental health professionals, by virtue of their position within an organization’s administrative structure or their roles in certain operations, will face enormous challenges in refusing to support or participate in actions that are deemed unlawful or lawful (under relevant bodies of law) but that violate their professional ethics.
For more information see:
https://www.amha-or.com/ethical-principles-practice-and-business-operation-for-mental-health
How Can Healthplans Successfully Contract and Implement MBC?
To implement MBC Health plans must recognize and overcome objections raised by psychotherapists. In what ways do psychotherapists resist and oppose the use of MBC?
1. Psychotherapists are expected to function as security officers and are ultimately responsible for patient privacy and confidentiality.
Security breaches are more common than published.
Psychotherapists are not experts in HIPAA security. Security professional are the experts.
Psychotherapists are responsible for electronic health record security, not Healthplans and vendors.
Psychotherapists are risk averse.
Psychotherapists believe the best way to manage risk is to have as few electronic interactions as possible.
2. Providers believe psychotherapy is patient centric. Some psychotherapists believe their patients….
Are not interested in measurement.
Have symptoms and functional problems that are not being measured in typical MBC measures.
Are different from patients treated by other providers.
3. The historical purpose of utilization review is unjustified and harms the public. Psychotherapists believe:
Utilization review does not improve quality or reduce waste. Those processed cause harm,
Healthplans will use measurement to restrict and direct care provided, and Healthplans cannot be trusted i.e., “Katie Bar the Door.”
4. The workflow of psychotherapy practice is such that psychotherapists always have a backlog of tasks. Priority dilution is a psychological process in which a people shift their attention to the more pressing, important, or rewarding task. The workflow of a psychotherapist is such that they must move to the next appointment or shift their attention to the next more important priority, leaving less urgent measurement priorities incomplete. Administrative and interactive complexity requirements in psychotherapy practice are:
Billing and authorization of services.
Record requests.
Maladaptive communication (related to, e.g., high anxiety, high reactivity, repeated questions, or disagreement that complicates delivery of care).
Psychotherapist emotions/behavior that interfere with implementation of the treatment plan.
Patient behavior or disclosure of event that requires consultation, report to a third party, and/or discussion of the event with relevant parties
Technical support for problems with EHRs, electronic MBC platforms, telehealth, and other devices.
MRI believes there are 3 important issues to implement MBC:
The measures used must have a high degree of face and content value. The content must be useful and of interest to patient and provider. Questionnaires that enhance the experience of therapy must be included with clinical screening, progress, and outcome measures. Psychotherapists need to feel the process of measurement has value in order to genuinely express that measurement will be helpful to patients. Patients must see the validity and value on the face of it.
The decision to shift priorities between appointments from a focus on relationship to measurement technology must be rewarding. The reward must be paired closely to the tasks. A financial reward for any action and the anticipation of gaining information that is useful is rewarding. It is also respectful of the psychotherapists time, memorable, ethical and a fortification against the distressing experiences and chronic conditions that psychotherapists encounter. A fixed ratio schedule of 1 is the most effective way to change dilution and choice behavior; and overcome the effects of procrastination.
Healthplans should contract with psychotherapists who are member of an incorporated group that can contract on behalf of members. This assures peer-based oversight for standards of practice, consultation, and administrative tasks.
To successfully contract for MBC, Moda must have a fee schedule that creates psychotherapists’ interest in participating in a Moda contract. MRI believes patients accept that psychotherapists want to provide quality care. Psychotherapists intend to provide quality care. However, psychotherapists, based on the history of their interactions with Healthplans, agree that Healthplans want psychotherapists to provide quality services, increase patient access, and for less money, which disproportionately profits Healthplans. Further, psychotherapists must safeguard their own mental health by restricting their caseloads and their case-mix severity. Payment which recognizes the difficulty of psychotherapists’ work, and their required practice efficiency is necessary if Moda hopes to improve outcomes and increase access to care.
Toward MBC that is Reliable, Valid, Useful and Valuable
MRI is excited to move forward with Moda to collaborate for ethical MBC. We have attached a recent JAMA article, a relevant synopsis of which might be something like: Moda has opportunity for innovation and use of routine systematic Behavioral Health measures by private practitioners, measures that can be shared when appropriate, with patients’ medical providers, and Healthplans.
By implementing a competitive reimbursement fee schedule and a pay-per-measurement model Moda will have all the data they need to calculate the ROI and the medical cost offset. Providers will gather and aggregate the data to make data informed decisions. This measurement-based model can evolve to provide programmatic, value-based contracts in Oregon for providers and behavioral health facilities.
References
Aafjes-Van Doorn, K. & de Jong. K (2022). “How to make the most of routine outcome monitoring (ROM): A multitude of clinical decisions and nuances to consider.” Journal of Clinical Psychology 78(1)
Britton, T. (2022) “Value-based Care in Addiction Treatment: Why it’s Essential and How we get There.” Addiction Professional, October 18, 2022.
Duncan, B.L., & Reese, R.J., (2015). The partners for Change Outcome Management System (PCOMS): Revisiting the client’s frame of reference. Psychotherapy, 52:4, 391-401.
Guo, T, et al (2015) Measurement-based care versus standard care for major depression: A randomized control trial with blind raters. American Journal of Psychiatry, 172:10, 1004-1013.
Howard, K. , C., Davidson, C., O'Mahaney, M., Orlinsky, D. & Brown, K. (1989) "Patters of Psychotherapy Utilization." American Journal of Psychiatry.
Howard, K. , Kopta, Krause, M., & Orlinsku, D. (1986). "The Dose-Effect Relationship in Psychotherapy." American Psychologist 41(2).
Kadera, S., Lambert, M., & Andrews, A. (1996).. “How much Therapy is Really Enough?” Journal of Psychotherapy Practice and Research.
Kopta, M., Owen, J., & Budge, S. (2015). Measuring psychotherapy outcomes with the behavioral health measure-20: Efficient and comprehensive. Psychotherapy, 52:4, 442-448.
Lambert, M.J. (2015). Progress feedback and the OQ-System: The past and the future. Psychotherapy, 52, 381-390.
Lewis, C. C, Scott, K., Marti, C.N., Marriott, B.R., Kroenke, K., Putz, J.W., Mendel, P., & Rutkowski (2015). Implementing measurement-based care (iMBC) for depression in community mental health: A dynamic cluster randomized trial study protocol. Implementation Science, 10:127.
Lewis, C.L., Boyd, M., Puspitasari, A., Navarro, E., Howard J., Kassab, H., Hoffman, M., Scott, K., Lyon, A., Douglas, S., Simon, G., & Kroenke, K. (2018). Implementing Measurement-Based Care in Behavioral Health: A Review, doi:10.1001/jamapsychiatry.2018.3329
Miller, S.D., Hubble, M.A., Chow, D., & Seidel, J. (2015). Beyond measures and monitoring: Realizing the potential of feedback-informed treatment. Psychotherapy, 52:4, 449-457.
Pincus, H. and Fleet, A. (2022) “Value Based Payments and Behavioral Health.” JAMA Psychiatry.
Robinsonia, L., Delgadilo, J., & Kellett, S. (2019).The dose-response effect in routinely delivered psychological therapies: A systematic review. Psychotherapy Research, (December 29)
Wampold, B.E. (2015). Routine outcome monitoring: Coming of age—With the usual developmental challenges. Psychotherapy, 52:4, 458-462.
Williams, A.R., et al. (2022). “Performance Measurement for Opioid Use Disorder Medicating Treatment and Care Retention.” American Journal of Psychiatry
Youn, S.J., Kraus, D.R., & Castonguay, L.G. (2012). The treatment outcome package: Facilitating practice and clinically relevant research. Psychotherapy, 49:2, 115-122.